As the Covid-19 pandemic loomed, the staff at one hospital in the English Midlands braced themselves. Quickly they found themselves at the centre of a coronavirus hotspot - and nothing turned out as they anticipated.
Liz Rees sat down at her dining room table to take the call. It was a Sunday in early March and, from down the line, a voice was telling her about some test results that had just come back from the lab.
This wasn't a normal diagnosis.
Image caption Liz ReesDudley, the town where Liz has worked for 20 years as a consultant microbiologist, had its first case of Covid-19. That, in itself, wasn't a surprise. She'd watched on TV as the virus had spread from Asia to continental Europe before reaching the south of England; it had already been detected in nearby Birmingham and Wolverhampton. "The was an inevitability about it," she says. "But the first one makes it real."
Liz's was the doctor in charge of infection prevention and control at Russells Hall Hospital in Dudley. She'd spent her career anticipating what to do in the event of a pandemic. And she knew the town - a one-time industrial powerhouse, the capital of the Black Country - intimately. Her husband joked she was attached to an elastic band that wouldn't stretch more than 10 miles out of Quinton, the nearby Birmingham suburb where she was brought up.
Still sitting in her dining room, Liz hastily convened an incident meeting over the phone with hospital staff. There was a list of things to check: That the patient was receiving the best possible care. That the staff on the ward were comfortable with what they were doing. Which infection precautions needed to be put in place.
The mood was calm. Everyone had a plan to follow. But this was uncharted territory. "I think we were aware that we would probably be getting more cases within days," says Liz.
For some time now, a Yorkshireman named Paul Hudson had also been anticipating that the outbreak would reach Dudley - and thinking hard about how to respond. But the first case came as a shock: "It wasn't from somewhere we expected."
Paul's job was divided in two. He spent half his time as consultant anaesthetist at the hospital, a role he'd occupied since 2009, and the other half as deputy medical director of the trust that runs it.
Image caption Paul HudsonAs the virus approached, he'd been closely involved in planning what to do - drawing up new guidelines; working out how to "zone" new arrivals at the front door into Covid and non-Covid streams; setting up a respiratory emergency department; and making sure there was enough stuff - oxygen, personal protective equipment, ventilators, drugs and people.
"We had, I think, quite a good plan in place," Paul says. It was just a question of waiting for patients with severe respiratory symptoms to start showing up at the door.
But that wasn't what happened, at least not at first.
"All of a sudden, we had a patient - an in-patient - test positive," says Paul.
This individual was being treated for something else entirely, having been admitted before they started showing symptoms. There were protocols in place for dealing with a situation like this to stop the virus spreading - but it was a difficult start all the same.
"I think that set the tone for a lot of the next few weeks and months," says Paul. "That has been, I think, one of the themes of this illness - that it has been unpredictable."
Qadar Zada sat in his office at the hospital. He'd been born less than a mile away and never lived anywhere other than Dudley. And yet everything around felt new to him.
In January 2020, Qadar had started as deputy head of operations at the trust. Part of his job involved making sure medical staff had all the support they need to do theirs. He'd spent his career working in NHS management and felt he had a good idea of what had to be done. There was a problem, though - most of his colleagues were strangers to him.
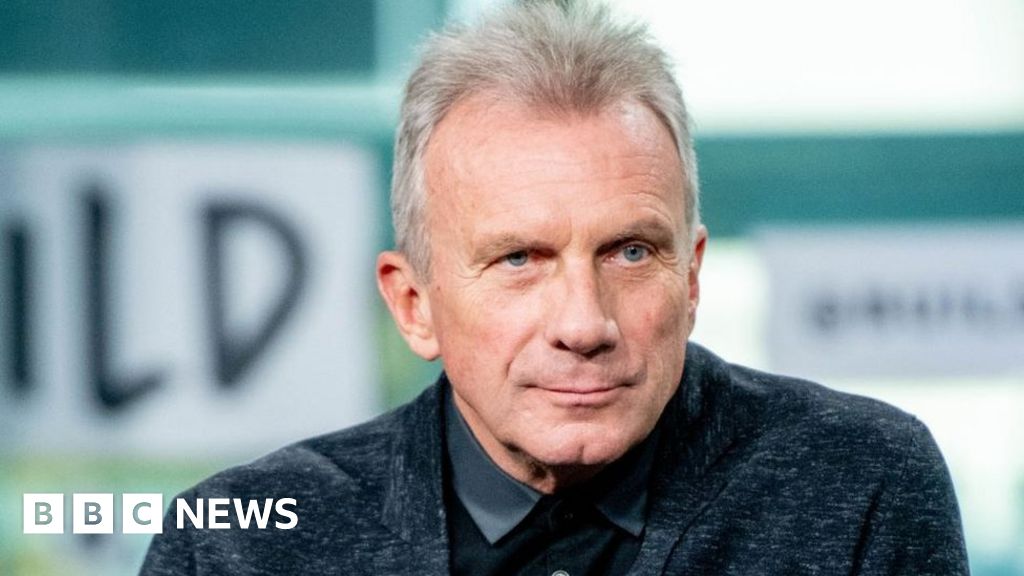
Image caption Qadar Zada"For me, I think the biggest challenge personally was that I didn't know people in the organisation," he says. The plan to give him a structured induction fell away. As the workload increased, no-one had time for a getting-to-know-you chat: "So at the point that we were talking to people about planning things, I was having to introduce myself."
There was also the duty he, a local councillor, felt towards his community. "I was worried, obviously, for those people in Dudley, family that I have in Dudley," he says. "I was worried for colleagues in the trust as well. But I was also aware of everybody's responsibility, including my own."
On 8 March, the day Tesco began restricting sales due to stockpiling and the UK Foreign Office advised against travelling to northern Italy, Dudley's first Covid-19 case was diagnosed. Three days later, the first fatality in the town attributed to the virus was reported in the local press. By 15 March the death toll stood at two, then rose to five by 18 March, then seven by the following day. On 20 March, Health Secretary Matt Hancock said the government was looking at why there was a "hotspot" across the West Midlands region.
According to Liz, the patients who died in the early days of the outbreak in Dudley were already very ill with underlying conditions. Typically, these deaths came rapidly after diagnosis. "By the time the result was back, possibly within 24 hours, they had died," she says. "It was clear at that point that this can be a really difficult disease to deal with."
For everyone at the hospital, all this was new. "People were learning what these patients look like when they came through the front door," says Liz. "The severity of the illness, and the breadth of people it could affect, was a bit of an eye-opener."
On the top floor of the administration block, a large office suite normally used for hosting seminars had been transformed. There were information boards around the walls and blinking computer monitors. A screen was tuned to the BBC News channel around the clock.
This was the trust's Covid incident room - a hub for all data coming in and going out of the trust.
"We were man-marking every single swab," says Qadar. The incident room received contact tracing information and produced situation reports throughout the day. There was also a PPE line for staff who needed personal protective equipment.
As well as carrying out its own modelling of how the virus might spread in Dudley, the trust was receiving projections from Public Health England, the local authority and other NHS agencies.
They warned how bad the impending peak could get. "At one point, the worst-case scenario, we were trying to plan for receiving up to 20 critically ill patients an hour for a number of days," says Paul. Back then, the hospital had just nine ventilated beds and another eight that offered advanced respiratory support. "That just doesn't work, do you know what I mean?"
On 23 March, the prime minister told the UK: "You must stay at home." Dudley joined the rest of the country in lockdown. At the same time, the surge in patient numbers everyone had been expecting was beginning.
Typically, "the people here are stoical and tend to present late - a salt-of-the-earth type thing", says Liz - but that wasn't the case any more. Covid patients were starting to turn up at the doors in large numbers, and a significant proportion of them were incredibly sick. According to Paul, those that weren't already acutely unwell when they arrived would typically deteriorate rapidly within days.
Between 23 and 25 March, the number of confirmed cases in the town jumped from 26 to 40. By 27 March, the number of Covid-related deaths stood at 17; four days later, that figure had nearly doubled to 30.
Around this time, a workaround for the concerns about ventilator capacity presented itself.
The trust had received guidance that a form of non-invasive ventilation called Continuous Positive Airway Pressure (CPAP) could be useful for Covid patients - either as a bridge to the usual mechanical ventilation techniques or as an alternative to them.
The Army had been drafted in to deliver essential supplies like PPE and oxygen to hospitals, and Paul recalls telling an officer - "I kid you not, his name was Major Tom" - that he worried the hospital was under-resourced when it came to CPAP machines. Soon afterwards a lorry turned up with 25 of them.
"And at that point, you could feel the mood around the place change a little bit," says Paul: it gave medical staff the confidence that they could take treatment decisions on the basis of patient need, not hospital capacity.
Ten operating theatres and a recovery area were transformed into a massive critical care facility, and the respiratory and high-dependency wards had been converted into a Covid-only CPAP unit ward.
It wasn't a moment too soon. The peak arrived in early April.
The parts of the hospital reserved for routine treatment were eerily quiet. According to Paul, "Our non-Covid work just fell off the edge of the cliff." But in the Covid zones, the pace was becoming frenetic.
By Sunday 5 April - the day the prime minister was admitted to hospital in London having already tested positive - the number of confirmed cases in the borough of Dudley had soared to 283. Three days later, it was announced that the number of hospital deaths stood at 106.
Liz recalls a single day in early April during which 58 new positive test results from the hospital came through, and not feeling particularly surprised by the number.
For most of that month, anaesthetic and critical care medics worked an intensive shift pattern - three long days, three days off, three nights, three more days off. Staff worked outside their comfort zones, carrying out tasks and working in departments that weren't part of their day jobs. Keeping rotas fully staffed became a huge challenge, not just for doctors and nurses but in every part of the hospital - at one point hundreds of employees were absent, either because they had fallen ill themselves or they were following advice to self-isolate.
The pressure faced by these front-line workers was unprecedented, says Paul.
"Trying to shout through the mask at people you barely recognise because you can only see the strip of their eyes - while the patients were incredibly sick and prone to very acute deterioration," he says. "You think you're making progress - and all of a sudden, they'd have these surges of deterioration where for the next four to six hours you're just trying to hold the tide back."
The prohibition on visiting made the task even harder, he adds: "Not having the relatives there to communicate with properly, and having to do everything shouted through a mask down the phone - I think it made it very, very, very difficult for a lot of our staff."
"All your decisions are a little bit more demanding," recalls Liz. "Your life has become a very narrow spectrum because the world's shut down around you. So either you're at home, or you're at work, and when your work is like mine.... I got to the point where I stopped listening to the news because I'd been dealing with it all day." To add to the breakdown in boundaries between her home and professional lives, Liz's daughter was working on a Covid ward in Sheffield as a junior doctor. "It's been a family business," she adds dryly.
The hospital never ran out of PPE - the trust, aided by the dedicated phone line in the incident room, did its job. But the local community played a crucial role, too, in preventing stocks from running out. "At one point, volunteers were making visors because we couldn't get any," says Qadar. One consultant surgeon helped source acetate for the front of them with the help of his daughter, a teacher, who regularly ordered it for classroom supplies.
"At one point I was wearing a pair of goggles donated to us by the chemistry department at a local school," says Paul. "One of my colleagues had a welder's mask, which looked really great - it was a kind of a mirrored black lens that was slightly less helpful when trying to look after people, because you couldn't see through it."
One evening, Paul turned up for a nightshift to discover there were no new Covid patients. Then the following night, there wasn't another patient either. And then a few days passed without any more.
The hospital staff could start to believe that the peak had passed.
Planning the recovery stage would be the next challenge. The non-emergency workload began to climb again, too. And everyone was well aware they needed to prepare for the possibility of subsequent spikes in infections.
But as the regular Thursday night clapping ritual drew to an end, they were able to take satisfaction in what they had achieved.
"You can look back and actually see that while what was done was really, on reflection, quite amazing actually," says Liz. "I think there's still a little bit of fear in the background about a second wave. But I think having done it once before, I think we know what we need to do."
Follow @mrjonkelly on Twitter
All photos by Tom Maddick/SWNS
You may also be interested in...
Image copyright Getty ImagesEarly in the Covid-19 outbreak, the Shetland Islands were one of the worst-hit areas of the UK by head of population. Now, no new cases have been detected there for six weeks. Some experts say it offers the rest of the country a route map out of lockdown - but for the first family on the islands to test positive, it hasn't been easy.
A cluster of islands: How Shetland locked down early and stopped the virus in its tracks

 5 years ago
637
5 years ago
637